Muscular Dystrophy Canada is the single largest funder of neuromuscular research in Canada. We are committed to advancing research that will unlimitedly lead to cures for neuromuscular disorders. One critical area is building research and clinical capacity by investing in the next generation of researchers and clinicians with expertise in neuromuscular disorders. Muscular Dystrophy Canada has partnered with the Neuromuscular Network for Canada (NMD4C) to launch two competitions this year to award funding for Postdoctoral Research Fellowships as well as Clinical Fellowships.
If you would like to receive notifications about clinical and research opportunities, please email research@muscle.ca
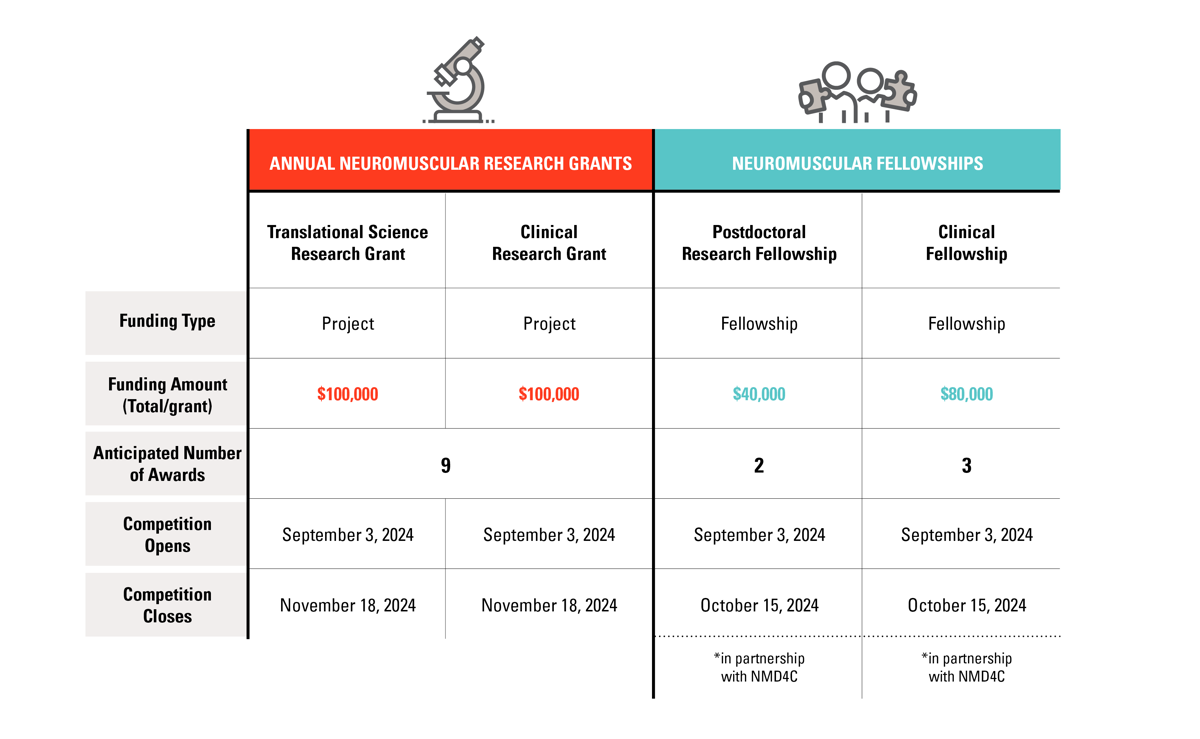
2025-2026 Neuromuscular Fellowship Deadlines:
Competition dates to come
- Competition Opens: September 3, 2024
- Competition Closes: October 15, 2024
- Decision Results Released: January 2025
See also:
2022-2023 Fellowship Recipients
All Funded Research Grants
Guidelines
2024-2025 Recipients
Clinical Fellowship Recipients
 Name: Dr Bridget Mulvany-Robbins
Name: Dr Bridget Mulvany-RobbinsTraining institution: University of British Columbia, Vancouver, BC
Supervisor: Dr Shahin Khayambashi
Budget: $80,000
Disorders: All Neuromuscular Disorders
Bio: Dr Bridget Mulvany-Robbins completed an undergraduate degree in Neuroscience, followed by medical school and neurology residency at the University of Alberta. Throughout her residency, she became drawn to neuromuscular medicine for its variety, nuanced clinical assessments, and rapidly evolving landscape. She is excited to join the University of British Columbia to complete her fellowship in Neuromuscular Medicine and Electromyography with support from the National Clinical Fellowship award.
 Name: Dr Annie Zhu
Name: Dr Annie Zhu
Training institution: University of Toronto – Citywide Neuromuscular Fellowship, Toronto, ON
Supervisor: Dr Aaron Izenberg
Budget: $80,000
Disorders: All Neuromuscular Disorders
Bio: Dr Annie Zhu completed their medical degree and residency in Adult Neurology at the University of Toronto. During residency, she developed a passion for electrodiagnostics and neuromuscular medicine and hopes to integrate her passion for education and art in this field as well. She will complete the City-wide Neuromuscular Fellowship Program at the University of Toronto to acquire further expertise in treating neuromuscular disorders.
Post-doctoral Fellowship Recipients
 Name: Dr Pauline Garcia
Name: Dr Pauline GarciaResearch/Clinical Sites & Affiliations: Centre Hospitalier Universitaire Sainte-Justine, Montreal, QC
Title of project: Exploring Mitochondrial Dysfunction in Myotonic Dystrophy type I Muscle Stem Cells
Supervisor: Dr Nicolas Dumont
Budget: $40,000
Disorders: All neuromuscular disorders (cross-cutting), Duchenne/Becker muscular dystrophies, Myopathy-genetic
Research Areas: Cell-based modeling and screening, diagnostic tools, tissue bioengineering
Summary of Project: Myotonic Dystrophy type 1 (DM1) is a genetic disorder that weakens muscles over time and affects several organs. Muscle stem ells, which help repair muscles, don’t function properly in people with DM1, leading to poor muscle growth and healing. Fixing these stem cells could offer a new way to treat DM1, but this has not been studied much yet. Dr. Dumont’s lab discovered that muscle stem cells in DM1 also have problems with their energy production. Mitochondria, often called the cell’s “powerhouses,” are essential for providing energy and regulating other important functions. When mitochondria don’t work correctly, it can cause many issues that could explain what is seen in DM1. Our project aims to explore whether malfunctioning mitochondria are behind the problems with muscle stem cells in DM1. We developed a 3 part plan to: First, study how badly mitochondria are affected in muscle stem cells. Then, find out what causes these defects in DM1. In a last part, investigate how these defects impact muscle healing. We’ll also test if certain drugs can fix the mitochondria and improve muscle stem cell function, which could lead to new treatments. We have the tools, human tissue samples, and animal models needed for this research. There is unfortunatly no cure for DM1, and patients have limited options to manage their symptoms or slow the disease’s progression. We aim to develop more effective treatments thanks to our work on mitochondrial dysfunctions in MuSCs.
 Name: Dr Tatiana Koeke
Name: Dr Tatiana Koeke
Research/Clinical Sites & Affiliations: Centre Hospitalier Universitaire Sainte-Justine, Montreal, QC
Supervisor: Dr Nicolas Dumont
Title of project: Targeting defective Muscle Stem Cells to treat Myotonic Dystrophy Type 1
Budget: $40,000
Disorders: Duchenne/Becker muscular dystrophies
Research Areas: Gene targeting therapy including gene transfer/ antisense oligonucleotides and gene editing, in vivo models, outcome measures for neuromuscular diseases
Summary of Project: DM1 is a multi-systemic disease that affects skeletal muscle. It causes muscles to weaken, shrink, and become stiff, making it hard for people with DM1 to move and do everyday tasks. This can make life much more difficult for them. The skeletal muscle tissue is composed of muscle stem cells that help the muscle grow and repair. Our previous study showed that the muscle stem cells of people with DM1 start to show signs of early aging. In this context, our research is focused on finding new ways to treat these damaged muscle stem cells. We believe that using senolytic drugs, which can remove aging cells from the body, might help improve muscle function. Exercise has also been shown to have similar effects as senolytics by getting rid of aging cells. We plan to investigate if combining senolytic drugs with exercise can reduce the number of aging cells and improve muscle health. To test this, we will examine muscle samples from DM1 patients before and after a 12-week strength training program. Additionally, we will study muscle tissue from mice with DM1 after they have exercised for six weeks. Our goal is to see if exercise and senolytic drugs together can repair muscles better than using them separately. By the end of our research, we hope to find effective treatment options that could lead to better therapies for people with DM1.
 Name: Dr Emma Sutton
Name: Dr Emma Sutton
Research/Clinical Sites & Affiliations: Ottawa Hospital Research Institute, Ottawa, ON
Supervisor: Dr. Rashmi Kothary
Title of project: Maternal transfer of an adeno-associated viral vector: a novel, minimally invasive approach to deliver SMN-gene therapy in Smn2B/- mice
Budget: $40,000
Disorders: Duchenne/Becker muscular dystrophies
Research Areas: Gene targeting therapy including gene transfer/ antisense oligonucleotides and gene editing, in vivo models, outcome measures for neuromuscular diseases
Summary of Project: We aim to find a new way to treat Spinal Muscular Atrophy (SMA) in babies before they are born. At the moment, all treatments are given to babies after they are born, but we want to see if treatment can work better if we give it to the baby’s mother while she is pregnant. To figure this out, we will use mice with SMA to see if giving a therapy to the mother can stop the disease from causing problems in the baby’s brain, spine, and muscles. If this research works, it could mean that treating the mother with a therapy before the baby is born might be a new and better way to use therapy for SMA.
2023-2024 Recipients
Clinical Fellowship Recipients
 Name: Dr Yiu-Chia Chang
Name: Dr Yiu-Chia ChangResearch/Clinical Sites & Affiliations: University of Western Ontario, London, ON
Budget: $80,000
Disorders: All Neuromuscular Disorders
Bio: Dr Yiu-Chia Chang studied Microbiology and Immunology at McGill University. He then obtained his medical degree at University of Ottawa and matched to Western University for residency training in neurology. During his residency, he developed a keen interest in neuromuscular medicine early on and took on extra rotations in the neuromuscular clinics and EMG lab. Among different sub-specialties within the neuromuscular field, Dr Chang is particularly interested in muscle diseases. During his fellowship, he aims to expand his knowledge and skills in the management of neuromuscular diseases and electrodiagnostics, as well as to acquire expertise in muscle diseases. He also aspires to be involved in medical education, with the goal of offering well-organized curriculum in neuromuscular medicine for trainees.
 Name: Dr Mark Krongold
Name: Dr Mark Krongold
Research/Clinical Sites & Affiliations: University of British Columbia, Vancouver, BC
Budget: $80,000
Disorders: All Neuromuscular Disorders
Bio: Dr Mark Krongold completed a bachelor’s degree in Neuroscience at the University of Calgary and medical school at Western University. He is currently completing his neurology residency at the University of Manitoba. Through his experiences in neurology, he developed an interest in electrodiagnostics and neuromuscular medicine. He looks forward to pursuing a career filled with constant learning and the chance to have a positive impact on patient’s lives. With support from the National Clinical Fellowship in Neuromuscular Medicine & Electromyography he will join the University of British Columbia for training in the upcoming year.
 Name: Dr Bram De Wel
Name: Dr Bram De Wel
Research/Clinical Sites & Affiliations: University of Calgary, Calgary, AB
Budget: $80,000
Disorders: All Neuromuscular Disorders
Bio: Dr Bram De Wel obtained his medical degree and completed his residency in neurology at the University Hospital Leuven in Belgium. During his residency, he obtained a PhD in neuromuscular diseases with a focus on advanced outcome measures in spinal muscular atrophy and muscular dystrophies. Dr De Wel will complete a neuromuscular medicine and EMG fellowship at the University of Calgary.
Post-doctoral Fellowship Recipients
 Name: Dr Yassine Ouhaddi
Name: Dr Yassine OuhaddiResearch/Clinical Sites & Affiliations: Centre de recherche du CHU Sainte-Justine, Montreal, QC
Title of project: Using 3D human iPSC-derived skeletal muscle modelling to elucidate the molecular mechanisms and develop new therapies for satellite cell-opathies
Budget: $40,000
Disorders: All neuromuscular disorders (cross-cutting), Duchenne/Becker muscular dystrophies, Myopathy-genetic
Research Areas: Cell-based modeling and screening, diagnostic tools, tissue bioengineering
Summary of Project: Skeletal muscles are essential to many physiological functions; yet, because myopathies are rare and heterogeneous, diagnosing and treating them can be quite difficult. This project presents an innovative approach to advance the understanding of satellite cell-opathies, a unique group of illnesses that affect the function of muscle stem cells. This project will use muscle cells and 3D tissue engineering to test the effect of rare genetic variations linked to satellite cell-opathies on myogenic cell function. This project aims to provide insight into the molecular pathways underlying these disorders and pinpoint possible targets for treatment. This project not only lays the groundwork for investigating secondary satellite cell-opathies, which will advance our understanding of the role of muscle stem cells in disease progression, but it also holds potential for offering patients with satellite cell-opathies individualized therapy options.
 Name: Dr Cedric Happi-Mbakam
Name: Dr Cedric Happi-MbakamResearch/Clinical Sites & Affiliations: SickKids Hospital, Toronto, ON
Title of project: Correction of intra-exonic insertions and deletions in DMD gene using CRISPR-Cas9 technologies
Budget: $40,000
Disorders: Duchenne/Becker muscular dystrophies
Research Areas: Gene targeting therapy including gene transfer/ antisense oligonucleotides and gene editing, in vivo models, outcome measures for neuromuscular diseases
Summary of Project: Duchenne muscular dystrophy (DMD) is a severe X-linked recessive disorder arising from mutations in the DMD gene, encoding the dystrophin protein. While the most common mutations involve the deletion of single or large exons, intra-exonic insertions and deletions represent approximately 3% of DMD mutations. This study will examine genetic mutations in patient myoblasts, mouse models and in vivo investigations to design and evaluate a CRISPR-Cas9 nuclease. The most efficient design will be selected and tested on a humanized mouse model. This research serves as proof of concept, and it holds promise to be adapted for other hereditary diseases sharing similar mutational profiles.